Cancer remains one of the most pressing health challenges worldwide. With nearly 10 million deaths attributed to cancer each year, it ranks among the leading causes of death globally.
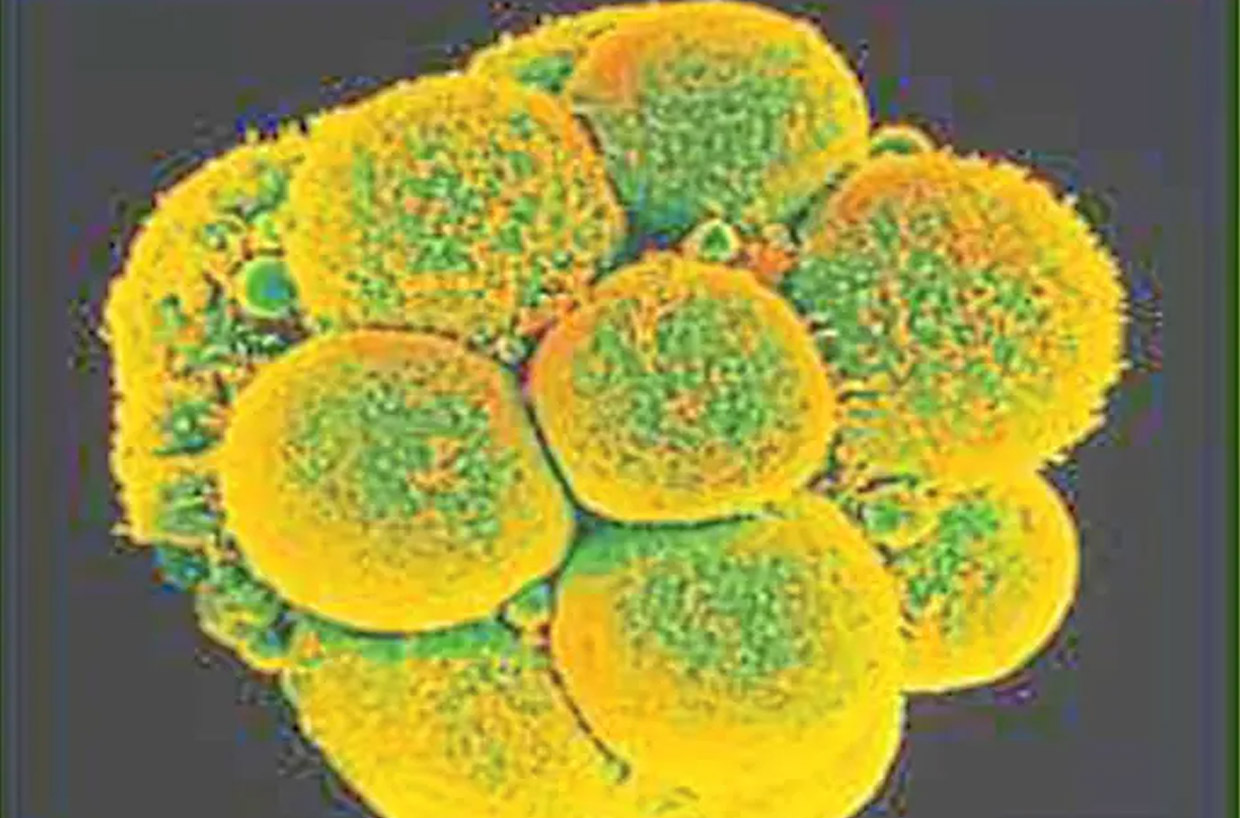
This chronic condition is characterised by the uncontrolled growth of invasive cells that can lead to the formation of tumours, as well as its propensity to spread to other parts of the body (i.e. metastasis). Common characteristics shared by different cancer types include genetic instability and the tendency for metastasis, making it a multifaceted health issue that requires thorough investigation.
While it is not traditionally classified as a metabolic disorder, there are significant metabolic changes that occur in cancer cells. This metabolic reprogramming that cancer cells undergo allows them to adapt their energy production methods to support their rapid growth.
The ability to thrive in low-nutrient and low-oxygen environments is crucial for cancer cell survival and proliferation. Gaining insights into this connection is essential for developing targeted therapies that can improve treatment outcomes for patients.
Connecting cancer and metabolism
A defining characteristic of cancer cell metabolism is the shift toward aerobic glycolysis, commonly referred to as the Warburg effect. Unlike normal cells that primarily utilise oxidative phosphorylation for energy production (which requires oxygen), cancer cells preferentially use glycolysis, even in the presence of oxygen.
This shift enables them to produce adenosine triphosphate (ATP) rapidly and synthesise critical macromolecules. ATP is the main molecule used to store and transport energy in our cells. Byproducts of aerobic glycolysis, such as lactate, can create an acidic microenvironment that further promotes tumour growth.
In addition to glycolysis, cancer cells employ alternative metabolic pathways, including fatty acid oxidation and glutaminolysis, to generate energy and the building blocks essential for cell division. Their ability to adapt their energy production mechanisms significantly contributes to their survival under various conditions.
The metabolic reprogramming observed in cancer cells also has profound implications for their growth and division. The reliance on glycolysis ensures a continuous supply of the biomolecules required for DNA (deoxyribonucleic acid), RNA (ribonucleic adic) and protein synthesis, facilitating the hallmark feature of cancer: unchecked cellular proliferation.
Furthermore, this change in metabolism affects key signalling pathways, particularly the mTOR (mechanistic target of rapamycin) pathway. This essential cellular signalling pathway governs cell growth, proliferation, metabolism and survival by integrating signals from various environmental factors such as nutrients and growth factors, and is closely associated with the availability of nutrients and energy.
Dysregulation of mTOR in cancer cells can drive tumour growth, highlighting the interplay between metabolism and cellular signalling in cancer progression.
Lifestyle choices in cancer metabolism
The interplay between diet, lifestyle and cancer metabolism is crucial to understand the development and progression of this disease. Our lifestyle choices can influence cancer-related metabolic pathways:
> Nutrition
Diet plays a significant role in shaping the metabolic landscape of cancer. Foods rich in nutrients, such as fruits, vegetables, whole grains and healthy fats, are associated with a reduced risk of cancer due to their antioxidant properties. Conversely, diets high in processed foods and sugars can lead to metabolic dysregulation, increasing cancer risk. Specific dietary approaches, such as ketogenic diets or caloric restriction, may also impact cancer metabolism and tumour growth.
> Physical activity
Engaging in regular physical activity is essential for maintaining metabolic health. Exercise enhances insulin sensitivity and reduces inflammation, both of which are beneficial in lowering cancer risk and improving treatment responses. Incorporating physical activity into daily routines is vital for both the prevention and management of cancer.
Obesity, which can be influenced by both diet and physical activity, is a significant risk factor for various types of cancer. This is largely due to metabolic alterations triggered by this condition that promote tumour development. Adipose tissue produces hormones and inflammatory cytokines that can lead to chronic inflammation and insulin resistance, facilitating cancer progression.
Lifestyle modifications focused on diet and exercise can mitigate obesity-related cancer risks and enhance patient outcomes. Public health initiatives aimed at promoting healthy weight management are crucial for cancer prevention. In summary, the choices we make regarding diet and lifestyle have profound implications for cancer metabolism.
Nutritional strategies, physical activity and weight management are essential components for influencing cancer risk and progression. Integrating these lifestyle changes into cancer prevention and treatment plans is critical for improving health outcomes.
Innovative therapeutic approaches
As our understanding of the relationship between cancer and metabolism deepens, new therapeutic strategies are emerging to specifically target the altered metabolic pathways in cancer cells.
> Metabolic inhibitors
Metabolic inhibitors represent a promising class of therapeutic agents designed to disrupt the energy production pathways that cancer cells rely on. One notable example is 2-deoxyglucose (2-DG), which inhibits glycolysis and effectively starves cancer cells of energy.
Other inhibitors target enzymes involved in mitochondrial respiration or fatty acid synthesis, thereby limiting the metabolic flexibility of tumours. Recent clinical trials indicate that these metabolic inhibitors can enhance the efficacy of conventional therapies, such as chemotherapy and radiation, by capitalising on the unique metabolic vulnerabilities of cancer cells.
A key challenge remains in identifying specific metabolic weaknesses across various cancer types to develop more effective, tailored treatment strategies.
> Personalised nutrition
Personalised nutrition is becoming increasingly important in cancer management, by focusing on optimising metabolic health. By understanding an individual’s metabolic profile, healthcare providers can tailor dietary recommendations to enhance treatment efficacy. For instance, ketogenic diets, which are low in carbohydrates and high in fats, may be beneficial in inhibiting tumour growth.
Targeting specific micronutrients and phytochemicals can also support conventional therapies. Customised dietary interventions that consider the metabolic state, cancer type and treatment regimen may significantly improve patient well-being and treatment outcomes.
Promising pathway
Research in cancer metabolism is advancing rapidly, unveiling new insights into the metabolic reprogramming of tumours. Future investigations are likely to focus on uncovering novel metabolic targets, developing effective inhibitors and integrating metabolomics into clinical practice.
Metabolomics is the study of small molecules, known as metabolites, within a biological system, which can range from a cell to an organism. It holds the potential to identify biomarkers that can predict responses to therapy and inform treatment decisions.
Additionally, exploring the impact of the tumour microenvironment on metabolic pathways could lead to the development of innovative and more effective cancer therapies. Targeting metabolic pathways in cancer represents a potentially transformative approach to treatment, by possibly enabling the development of personalised therapies that cater to individual metabolic needs.
By continuing to explore the intricate relationship between cancer and metabolism, researchers and clinicians could pave the way for more effective interventions that ultimately improve patient outcomes.
By Datuk Dr Nor Ashikin Mokhtar
Published in Star Newspaper, 05 May 2025